In its second season, the Longevity & Aging Series is a video series that features esteemed researchers discussing the latest in aging research with a focus on their studies published by Aging.
—
Below is a transcription of the the third episode of Season 2 of the Longevity & Aging Series. Here, Dr. Jon Berner from the Woodinville Psychiatric Associates in Woodinville, WA, joins host Dr. Evgeniy Galimov to discuss a research paper he co-authored that was published in Volume 16, Issue 14 of Aging (Aging-US), entitled “mTORC1 activation in presumed classical monocytes: observed correlation with human size variation and neuropsychiatric disease.”
Welcome to the Longevity & Aging Series. Today I would like to introduce to you Jon Berner. Jon is a board-certified psychiatrist in solo practice at Woodinville, with 27 years of experience. He’s committed to promoting innovative treatments and his research interests are neural network stability with nonlinear internal feedback, neuropsychiatric consequences of altered cytosolic amino acid sensing, clinical characteristics of ketamine responders in pain and depression, and neuropsychiatric toxicity of drugs with mitochondrial targets. Dr. Berner recently published the paper titled, “mTORC1 activation in presumed classical monocytes: observed correlation with human size variation and neuropsychiatric disease.” But before we start discussing the paper, Jon, could you please tell us more about your background and how you became interested in this topic?
Sure. So, I’m a practicing psychiatrist. I was always interested in psychiatric disease as related to metabolism, rather than necessarily cell surface signaling, given personal experience prescribing lithium. Because lithium is a glycogen synthase kinase inhibitor, that presumably affects every cell in the body, and yet it has such a powerful effect in classical bipolar patients and what’s looking to be very true in terms of Alzheimer’s and other dementia prophylaxis.
There’s this concept that tissue is not defined by its cell surface activity, but it’s actually defined by the metabolism which underlies its function. And that’s a really powerful concept. So, I’ve always been interested in this area. And then in 2007, I started prescribing ketamine and have done a lot of the original work in that area. And it became clear with experience that the effect of ketamine on a daily usage, for many people, is related to its central anti-inflammatory effects.
Ketamine almost certainly changes the equilibrium distribution in the brain between the type I microglia, the pro-inflammatory microglia, and the M2c microglia whose promoters are typically IL-10 and corticosteroids, and are related to extracellular matrix modulation. And ketamine’s been a major advance in psychiatry, probably our biggest advance in the last 20 years. There’s an article in the Lancet describing 400 patients randomized to IV ketamine and ECT, who failed traditional therapies, and the response rate to ketamine was 55%. I mean, that’s amazing, across all branches of medicine, that we have something that’s this potent. And so, given that we have an effective treatment, how can we make it work better? How can we do dose finding? How can we improve patient selection? And that means we need to focus on the metabolism associated with the microglia. And obviously, doing brain biopsies in humans is challenging to say the least.
We’re left with the available tissue, which is the monocyte fraction in the blood. It’s not a perfect fraction because, for all sorts of reasons. I mean, number one, tissue-resident macrophages in the brain, the microglia come from the yolk sac in the embryo, and they are different tissues than the monocyte derived tissue-resident macrophages. And so, that’s a problem. And then the other problem is that, most of the monocyte fraction in the blood is actually stem cell. It comes out undifferentiated. And so, it’s not going to be easy to really focus in on what we’re interested in, which is the M2 like tissue-resident macrophage population in the blood.
There is an M2 macrophage population. It is designed to repair the endothelial cells in the arteries, from turbulent flow, from hypertension and from other sorts of issues. So, colony stimulating factor actually can induce the stem cell monocyte that’s floating around in the blood, to become a tissue-resident macrophage.
And I think that’s the theoretical idea behind the paper, which is, can we, with the grossest of assays, essentially we take the buffy coat fraction from the blood and look at a differentiated cell, a non stem cell. And look at that gross assay and correlate it with our clinical population and say, “Hey, is there information here that is potentially useful for clinical management?” And really, to our surprise, I mean this is the most pilot study you could possibly imagine, very small sample sizes, very few readouts. We actually saw findings that are consistent with the known biology and have been replicated with other groups.
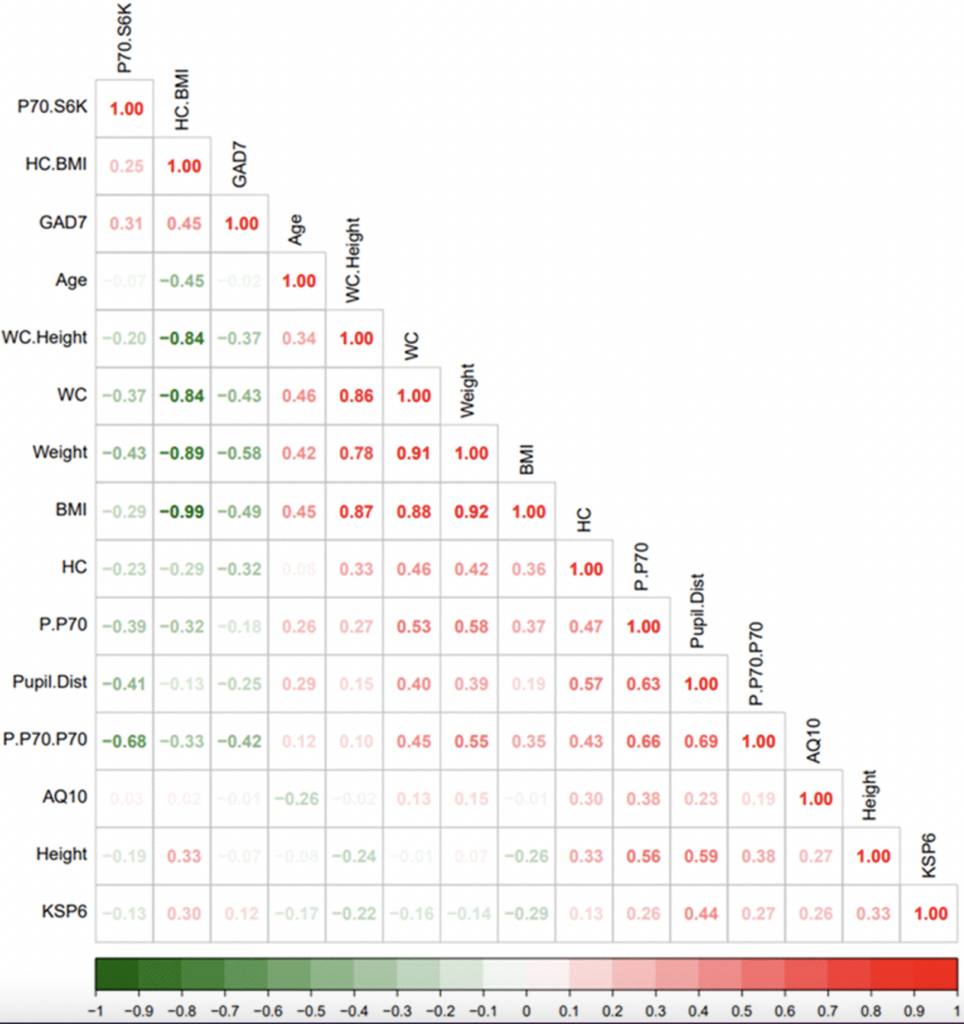
Essentially the study was, is we took buffy coat samples from 30 women who are in a psychiatric clinic. I mean, so these are not normal controls, these are clinical samples. And we looked at surrogate measures of TOR activation in that population, which would be phosphorylation of S6 kinase. And then we looked at how that sort of related to the phenotypic landscape in this population. And what did we see? One thing we saw, which we thought was extremely interesting, is that the phenotypic concept of macrocephaly, pupil distance and head circumference, correlated with S6 kinase phosphorylation.
And this has been described in animal models of P10 knockouts, where you see constitutive activation of TORC1 throughout a lifetime, that these animals tend to have very large heads. And if you use antisense RNA, you can reverse, only to TORC1, not to TORC2, you can reverse the macrocephaly. And so, we had some previous unpublished clinical data that suggested head circumference was a predictor of ketamine response. And this was sort of our, if you will, positive control. And we saw this and we said, oh my gosh, there’s so many ways to very reliably critique our lab technique. But we have a positive control in even a small sample size, and so, that provided us with a lot of confidence, we were seeing what we were hoping to see.
And when you say positive control, it means you see some confirmation that there is TORC1 activation in the blood?
Right. So in other words, the TORC1 inflammation elevation is not unique to the monocyte fraction. It’s a gain of function distribution within every cell in the body, because it shows up as macrocephaly in this population.
But in this paper, you just cited, does it mean that activation of mTOR is coming from nutrient sensing or there is some immune-related signaling, which leads to white blood cell activation of mTOR?
Okay. I think the concept is that, everything in biology is Gaussian, right? And we all live in a gradient. And there are people who are born with constitutive increased mTORC1 activation for all sorts of reasons. And there are people who are born with decreased mTORC1 activation for all sorts of reasons. And one of the phenotypic manifestations of elevated TORC1 activation is macrocephaly, is having a large head relative to the rest of the body. And that seems to be strongly implied by studies looking at P10 knockouts in rodents, that macrocephaly is a phenotypic variant of constitutive mTORC1 activation.
Basically the idea is then that, this patient with a depression, in your paper, they have somehow a high activation of mTOR, but this may be due to some constitutive increased activity of mTOR, which is reflected-
Throughout the body. It may not just be in a myeloid population, whether the myeloid population be the bone marrow-derived macrophage, or whether the myeloid population be the embryonic yolk sac tissue-resident self-renewing population in the brain. It may be throughout the entire body.
But do we really have the evidence that mTOR activated, if you see activation of mTOR, higher activity of mTOR, in blood cells, the same happens in all other cell types? Or do we really have the studies? I’m just like, I’m not sure I know the studies.
Well, right, it’s cited in the paper, the P10 rodent knockout paper. So, if this was a tissue-specific finding, we wouldn’t expect correlation with head size, but we did. And it was even in a relatively small sample, which is really, I thought quite interesting.
Okay, cool. And then you basically measure an activity of mTORC in white blood cells and want to predict ketamine response. Right?
Right. And what we saw in general is that, the more readout of TOR, phosphorylated S6 kinase, the more likely you are going to see a ketamine response.
But can you define, what do you call ketamine response? Because-
Oh, it’s simple. It’s a binary issue. Do patients want to take ketamine? So, when you work in a clinical setting, for people with chronic depression, it’s routine for them to try 5, 10, 15 agents, in order for them to see if they can improve their depression. And it’s really just a sequential sampling problem. It’s a search problem. And so, people simply don’t take drugs that don’t provide them benefit.
But in this case, by saying they want to take ketamine, it means they want to take ketamine after three doses, after two doses, after 10 doses?
This would be sustained over a period of months.
Okay. This isn’t a short-term placebo trial, this is… In general, when you give people in a randomized trial, these are six-week trials because the placebo effect lasts for three weeks and then it goes away. But in clinical practice, what you find is that, there’s a binary decision point. This drug clearly helps me, I’m going to pay to go to the pharmacy every three months to take a drug, because I’m finding benefit. And patients simply don’t take drugs that don’t work. I mean, not over periods of months. I mean, placebo effects are one thing, but that’s not what we’re dealing with here.
And then basically you used all these physical size measurements and phosphorylated S6 kinase to predict ketamine response. Right? And you used a random forest algorithm for that.
That’s correct. And again, this is a very small sample size. Obviously, we’re going to need a lot of high-quality, expensive, clinical work to expand on this paper. I mean, we did this on a shoestring, and this is clearly pilot data.
But what’s encouraging is, when we look at some of the other studies, I mean, what are you looking at? It looks like Still’s disease, which is chronic inflammation, chronic imbalance in the M1 pro-inflammatory tissue-resident macrophage population versus the reparative M2 macrophage population. To some degree, this defines this problem. If your tissue-resident cells are trapped in a glycolytic inflammatory phenotype, you’re not going to be able to induce the TORC2 fatty acid oxidation, reparative and trophic tissue-resident macrophage population. And there’s lots of roads to roam on this issue. This isn’t a one gene one disease phenotype knockout. This is a vector of forward and backward rate constants, which affect the population distributions of these different tissue-resident macrophage populations.

I just came across some COPD literature that did exactly the same protocol. I mean, it’s almost exactly the same. And they found the same finding in individuals with COPD. The individuals that had upregulated phosphorylated S6 kinase with COPD, had much higher levels than the normal controls. So, this may be relevant in disorders other than simply depression, but all sorts of issues related to tissue repair and barrier defense, rather than simple just depression.
But basically, for this particular paper, the way you interpret this is that, there is some differentiation of monocytes in the tissue-resident macrophages related on mTORC1 activation, right?
Right.
And can you tell more about the function of this tissue-resident macrophages in brain? Does it mean that basically they cross the brain-blood barrier, and do they become M1 or M2 subpopulation? And what is the role of these macrophages?
Oh, yeah. No, this is a great question, right. In the ideal world, you don’t want the monocyte fraction to cross into the brain. Because, the monocyte fraction, if it crosses into the brain, is recruited only in the context of severe tissue death. And it’s going to have epigenetic imprinting, and it’ll take months to years, to respond to niche signals and become the phenotypic equivalent to the tissue-resident embryonic macrophage. So, it’s really dangerous to have recruitment of the monocyte fraction into the brain, because it may take a long time for you to hit your normal distribution.
This is the problem with things like recurrent head injuries, and encephalitis is, the restorative population is there all the time, and its job is to digest synapses. The M2a population is phagocytic, right? So, its job is to digest synapses that are senescent. Presumably they have some, as a concept, they have mitochondrial damage, and they’re putting out too many damage-associated molecular patterns. They’re saying, “Hey, this synapse is sick, digest it.” And then the M2c population is supposed to repair the extracellular matrix, so there’s room for new memories to form within the brain. And this process is happening dynamically during sleep. So, there’s a lot of learning that goes on during the day. The blood flow to the brain increases by 30% over the day, as you learn new things, and your synaptic density increases and your synapse arbor grows.
But then, in order to avoid an overgrowth syndrome in the brain, you have to edit the hard drive. And the restorative M2 macrophages in the brain, the M2 microglia, that’s their job. And when that doesn’t work, you get Alzheimer’s disease. So, 50% of the defects in Alzheimer’s disease, are known to be defects in tissue-resonant microglia. It’s not necessarily simply a synaptic disease. It’s a disorder of tissue repair in 50% of the genetic loading.
But what percent of this microglia is obtained from during embryogenesis or after that? And what percent coming from blood, when you talk about adults?
I don’t do the original research in that area. But my sense is, if you do the fate mapping data, and that’s not my level of expertise, is all of it is embryonic. In the ideal situation, without brain injury, your stem cell population, there’s a unique bone marrow in the brain with a myeloid component that is there over a lifetime.
But when we measure white blood cells content of mTOR, activation from mTOR, it means, we think that, you know, when you say that some amount of the monocytes differentiate and become tissue-resident macrophages, does it mean that they go from blood through brain-blood barrier?
No, the tissue-resident macrophage in the blood, is designed to repair the endothelium. Right? So, if you have a defect in tissue repair in the endothelium, you develop atherosclerosis.
I’m just trying to connect, because your finding is that, you basically measure mTORC activity in the blood, right?
Yes.
But when you talk about depression and when you’re trying to talk about microglia effects, so basically you don’t measure microglia effects, you measure mTORC activation in the blood. So, how is it related to the ketamine effect on microglia?
The assumption is that the source code, the metabolic gain of functions, in the tissue-resident microglia, I mean the tissue-resident macrophage in the blood, which is repairing the endothelium, is similar to the source code gain of function to the microglia inherited gain of function. That they shares a common metabolic tendency, because they’re closely related. They’re not exactly the same. Right? The niche signals from the endothelium are different than the niche signals from the neurons and the astroglia. So, they’re not exactly the same, but they share a lot of commonalities. In terms of their damage-associated molecular pathway, processes, their excretory profiles, they’re about as similar as we’re going to get, other than doing a brain biopsy.
Well, basically my question is about, we see some correlation, but is there any causative link? How can we interpret this? Or it’s just basically, we just found some correlation for prediction, but you don’t really know the mechanism of how mTORC1 activation in white blood cells can actually explain the fact.
No, no, no, no. Remember, it’s all physical chemistry, right? Cells are just bags of chemicals. They have forward rate constants and backward rate constant. So, if TORC1 is too activated, by definition, a tissue-resonant macrophage is going to be in the pro-inflammatory state. And it’s not going to be in the TORC2 reparative, high fatty acid, oxidation state. You’re going to have a different population distribution. I mean, that’s just physical chemistry. These are equilibrium distribution. So, if you’re seeing too much TORC1, by definition, potentially you’re seeing too little TORC2, complete cell differentiation.
In other words, the fully differentiated monocyte is an M2. It has high levels of fatty acid oxidation, lots of processes that are extending out and monitoring the integrity of the local environment. And they do surveillance of the local tissue by sending out these processes that follow purine gradients, at least in the brain, looking for local cell damage. That’s the differentiated monocyte or the fully differentiated tissue-resident macrophage. When you become inflamed, you de-differentiate. You go back to the glycolytic form, which is mTORC1 mediated, and you excrete a lot of inflammatory cytokines.
Okay. So, basically, the way we can interpret this potentially that, this patient have higher level of inflammation.
Yes.
And basically, that’s why if we see the higher level of inflammation in the patients with depression, we could expect a better response for ketamine, because why? Because ketamine…
Because ketamine activates, forces … the ketamine is a central anti-inflammatory agent. In tissue experiments, and to some degree in vitro as well, in vivo as well. Ketamine induces tissue-resident macrophages to move from an M1 phenotype or from a stem phenotype, an M0, into an M2c phenotype. And it decreases the equilibrium distribution of the M1 phenotype. So, from clinical practice, many rheumatologists will look for markers of systemic inflammation, C-reactive protein or sed rates, and they’ll say, “Hey, look, you’re clearly inflamed.” The argument that we’re making is that, you can see the inflammation actually within the tissue-resident macrophage population, and that predicts whether or not you’re going to have central inflammation. So, if you see inflammation within the tissue-resident macrophage population in the blood, it’s going to predict that you also have central inflammation in the brain and that you’re going to respond to ketamine.
The concept is, ketamine is not a classical psychiatric drug. It’s not an upper or a downer, right? It’s actually anti-inflammatory.
But what we know about the effect of ketamine on neural system, because my understanding about ketamine when I read it was that it affects inhibitory GABAergic interneurons.
Right. Well, ketamine binds a lot of places. Right? And so, what everyone has noticed is that, when ketamine binds the NMDA receptor on the parvalbumin-positive interneurons, you get a disinhibition syndrome in the frontal lobe, and patients report these deliriums and sort of psychoactive experiences. The problem with the dogma is that, it’s simply not true. That you can treat patients with ketamine and cause absolutely no subjective delirium and no subjective increases in firing rates. And they have a very profound clinical response.
And I think this fits with the idea that the NMDA receptor is… Ketamine’s binding a lot of places in the brain, And there may be some people that respond to the disinhibition pulse… And I can go into that, but that’s beyond the scope of this discussion.
But there’s a high proportion of patients, maybe even dominant, that the central effect of ketamine is on microglia. And this has been known in the chronic pain world for 25 years. People get ketamine comas in Mexico where they’re unconscious for 24 hours or people get hour-long infusions for chronic regional pain syndrome, and they have a very good response to ketamine, and it’s completely unrelated to the dissociative effect. So, I think psychiatry has gotten stuck in this concept of parvalbumin-positive response. They may be orthogonal processes, and we didn’t talk about that in the paper.
Thank you very much. It’s making it much clearer now, to me at least. And what are you going to do in future? Are you going to design a bigger study, involve more patients?
We’re kind pivoting into the rapamycin world, because it’s a little bit easier to find people to check our work. I find the ketamine world, in the psychiatry setting, to be really, to some degree, an intellectual wasteland. Everyone’s stuck with the concept of cell surface signaling, and microglia is still this tiny flicker of interest in the psychiatry world. I don’t see a lot of interest in this area. Whereas the rapamycin world, it’s very popular, a lot of flexible thinkers. And so, we’re trying to work hard in coming up with a way of understanding the combination of ketamine and rapamycin.
Since ketamine is inducing M2cs and rapamycin is inducing M2as, and then both of these drugs are inhibiting M1s. And so we really have an equilibrium distribution of three populations. The M1, the M2a, the M2c, they’re all in competition with each other. How do you do patient selection in this three-dimensional landscape? How do you do dose finding in this three-dimensional landscape? I mean, there’s not a lot of folks out there, who are able to put the resources together to do the high quality scientific work we’d like to do. That’s just sort of getting the word out that this is an important area, and waiting for the community to coalesce in this area.
Let’s maybe quickly talk about limitations of the study. You mentioned one of the limitation is that it’s done on females, but basically what do you see the effects on males would be?
Right. And males, I think the recent … men and women clearly have different gain of functions in their basic tissue macrophage activity. I mean, males are more, I think, related to tissue repair associated with dominance battles, TNF-alpha-mediated. And women are more maybe interferon modulated in terms of fetus defense during pregnancy. A virus infection during pregnancy is a problem. And so, it’s not surprising, you see pretty radical differences in the immune system between males and females.
And as someone who’s a psychiatrist, I mean, this is such a rich area. It’s going to be hard for me to really sketch out for other individuals about how to approach this issue. But that’s a problem. Right? I think the other problem is, we wanted to do more than one tissue type. We were planning on doing buccal tissue as well, and we just didn’t have the resources from our basic lab, from Alaattin’s group, to do the confirmatory studies across multiple tissue types. That obviously would be useful.
Well, I think one of the limitations is that, we really don’t know. Well, it’s a kind of speculation that it works on monocytes, because in the paper, it wasn’t shown clearly, right?
Oh, yeah. Oh, absolutely.
We really need… I think the next step would be selecting, maybe using cytometry. [inaudible 00:34:29]
We’d have to gate with this, and that’s very expensive and that’s- to some degree, that’s both beautiful from a scientific perspective, but also perilous from a rapid consumer adoption perspective. But ultimately, what we want is something really cheap and really easy to get, so that we can put this out for patient use as fast as possible. Because, the big science problem is just such a huge problem, right? We have these beautiful data that’s replicated, but there’s only 5 or 10 groups around the world that have the money to do this expensive gating technologies. And then it takes another five years to get it replicated, it takes another five years to get it replicated. And everybody’s completely confident about it, but by the time we have that confidence, nothing gets done. I’m making this argument, hey, sometimes a little bit of noisy data is really good, because you can replicate it with a thousand people, rather than five groups. And I think there’s something to be said for that. Do we want to replicate with really clean data or do we take terrible data and just bootstrap it?
Yeah. No, obviously simple tests would work better for this kind of investigations. Well, Dr. Berner, thank you very much for providing insights and explanation for this paper. It’s cool that we now have more advanced techniques to predict ketamine response, and hopefully it’ll be in fast speed development soon. Thank you.
You’re welcome. Thank you very much.
All the best.
Bye.
Click here to read the full research paper published in Aging.
—
Aging is an open-access, traditional, peer-reviewed journal that publishes high-impact papers in all fields of aging research. All papers are available to readers (at no cost and free of subscription barriers) in bi-monthly issues at Aging-US.com.
Click here to subscribe to Aging publication updates.
For media inquiries, please contact [email protected].