Below is a transcript of an interview with Senior Researcher Dr. Julija Juric detailing the research of the Genos Glycoscience team that was published by Aging (Aging-US) on October 13, 2020, entitled, “Effects of estradiol on biological age measured using the glycan age index.”
Behind the Study is a series of transcribed videos from researchers elaborating on their recent studies published by Aging (Aging-US). Visit the Aging (Aging-US) YouTube channel for more insights from outstanding authors.
—
Hi, my name is Julija Juric. I’m a Senior Researcher at Genos Glycoscience company, one of the world’s leading laboratories in high-throughput glycomics. My field of expertise includes sex hormones and glycans, which are interconnected with aging processes in women. I would like to use this opportunity to present you with a paper that we recently published in a journal Aging. This paper describes how estrogen affects biological age in women, and that we measured using the glycan age index. This was a study done with the help of our collaborators from the United States, Professor Wendy Kohrt and a medical doctor, Peter Nigrovic.
So glycan age is a recently developed biomarker based on glycans, which are actually short sugar chains attached to immunoglobulin gene antibodies. So back in 2014, we performed a large cohort study based on glycans that showed us that the composition of glycans on antibodies change with lifetime, and could be actually used to predict pharmacological age.
However, for some people, their chronological age was very much different than the age that was estimated using the glycan age index, and this was usually associated with unhealthy lifestyle or some disease risk biomarkers. At that point, we realized that the glycan age actually shows how healthy the immune system is, and this could be ideal for estimating person’s biological age. So as we conducted more and more glycan analysis, we realized that the most pronounced changes occur in women around their 50s. So it is the time when women enter menopause and experience a sharp drop in the level of sex hormones, especially estrogen. It is also the time when they often develop autoimmune diseases, which are associated with enhanced inflammatory function of antibodies because of the increased abundance of some special glycan structures attached to those antibodies. So in the research that we published in the journal Aging, we explored how important is the level of sex hormones, specifically estrogen for the glycosolation of IgG antibodies.
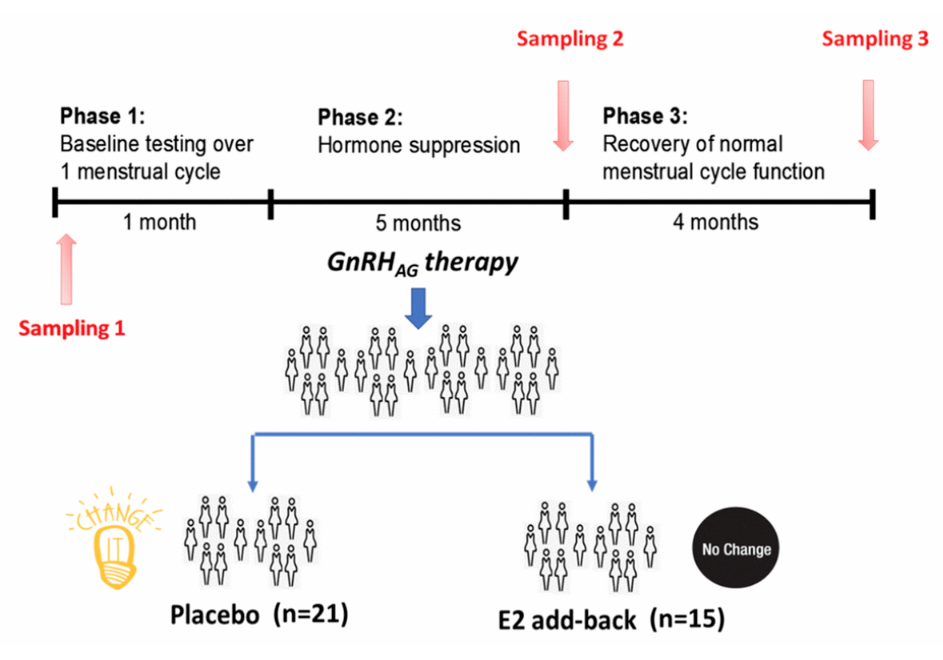
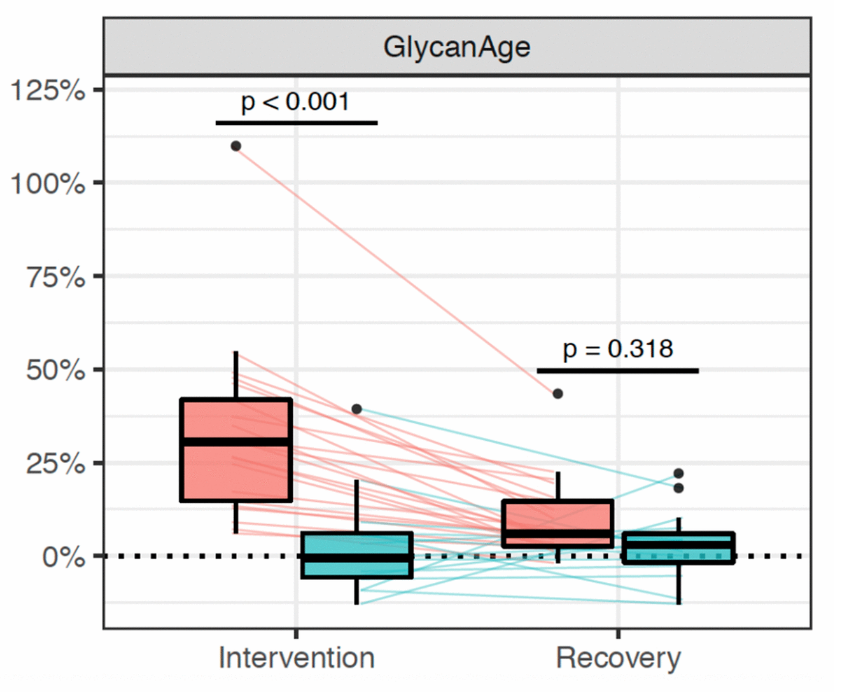
First, we used medications to chronically suppress the production of sex hormones in the ovaries of women. They were healthy and young, having regular menstrual cycle. During this period, one group of participants received estradiol supplementation, and the other group received placebo, which kept very low levels of sex hormones in their plasma as if they were in menopause. So the question here was: Will the lack of sex hormones in this case cause changes in glycans? And if the answer is yes. Will this affect the glycan age? So to answer these questions, we analyzed IgG glycans in women before and after the intervention, and we saw that placebo women had their glycan age increased for nine years. So within six months of intervention, so medically induced menopause, women became on average nine years older than before the intervention. We actually didn’t see, and it didn’t happen in women who received estradiol.
So this showed us that IgG glycans, as well as glycan age are under strong influence of sex hormones, especially estrogen, and that estrogen therapy could prevent the increase of glycan age that happens in perimenopause. And this discovery actually led us to another exciting research, and the results are about to be published. So they’re not published yet, and you are having an exclusive.
So besides aging, women in menopause more often develop rheumatoid arthritis. That is one autoimmune disease, and they actually have a higher risk of developing cardiovascular diseases. But the good thing is that we realized that we could track changes in glycans many years before the disease develops and based on those changes, we can stratify people with a higher risk of developing such diseases, and this opened a whole new area for us. So our main idea was to use glycan age as a biomarker to detect those bad changes in a person and try to prevent disease development.
This would be a part of the personalized health monitoring, which would include men and women from their reproductive years on. But then we faced another problem because for women, it meant that glycan age could be influenced by fluctuating levels of sex hormones during their menstrual cycles, and the data on such glycan changes still did not exist. So with the help of our collaborators from Australia and from China who provided samples, we set up the study on a group of healthy young women and actually analyzed their antibody glycans at 12 time points along their menstrual cycles. We tested them every seven days during three months, regardless of their menstrual cycle phase. What we saw was very interesting. We saw that glycans change periodically during the menstrual cycle, and that those changes can be associated with menstrual cycle phase and the concentration of sex hormones in plasma.
The menstrual cycle starts with menstrual bleeding. This is initiated by low level of sex hormones, and our study showed that women have increased abundance of glycans that promote inflammatory antibody action during this period. While after the ovulation, a high concentration of estradiol and progesterone remotes such glycan changes that make antibodies act anti-inflammatory. So in general, our research showed that these changes are minor, but in some individuals they were relatively common, which means that women’s immunity really does change during the menstrual cycle. This is a very important discovery of our research, which is not only important for future epidemiological studies on the disease etiology, but can be useful in many other applications where sex differences in immunity are crucial like vaccination strategy, or therapy regimen for autoimmune diseases, or some other chronic diseases in women in their reproductive years, as well as for the longitudinal health monitoring with glycan age biomarker, which actually still needs to be further explored.
I want to acknowledge all our former collaborators and welcome all our future collaborators in new, exciting research in the field of glyconics.
Thank you from the whole Glycoscience group in Croatia. Bye.
Click here to read the full research paper published by Aging (Aging-US).
WATCH: AGING VIDEOS ON LABTUBE
—
Aging (Aging-US) is an open-access journal that publishes research papers monthly in all fields of aging research and other topics. These papers are available to read at no cost to readers on Aging-us.com. Open-access journals offer information that has the potential to benefit our societies from the inside out and may be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact [email protected].
